infotx@cpt.eurofinsus.com |
(512) 243-6426
CONtact us to get a quote!
Introduction
One of the key components to take into consideration during product development is ensuring product safety. Antimicrobial preservatives are elements of formulations included to protect against microbial contaminants that may be inadvertently introduced during manufacturing or during use by the customer.
Preservatives used in formulations help to protect the consumer from exposure to contaminants as well as maintain the product’s integrity throughout its shelf life. Microbial contamination can affect a product’s aesthetics/appearance and odor, leading to product recalls that could have a detrimental effect on a brand’s equity.
The following test methods are used to determine the preservative robustness of a product formulation:
USP <51> Antimicrobial Effectiveness testing (ep and JP)
The most widely used method to evaluate the effectiveness of added antimicrobial preservatives to aqueous based products. Products are evaluated against 5 different microorganisms (3 bacteria, 1 yeast and 1 fungus) at two or more sampling intervals (commonly 14 days and 28 days, but may differ based on the product category). Based on the obtained from each sampling interval, a product either conforms or does not conform to the USP <51> acceptance criteria.
ISO 11930:2019 - Cosmetics - microbiology - evaluation of the antimicrobial protection of cosmetics
This ISO testing methodology intended to evaluate the overall antimicrobial protection of a cosmetic product that is not considered low risk, based on a risk assessment described in ISO 29621. Although the EU Cosmetics Regulation does not define a specific test method to be used for satisfying the requirements for antimicrobial robustness, the ISO 11930 is commonly recommended, especially for water soluble or water-miscible cosmetic products. While the test is very similar to the USP <51> testing methodology described above, ISO 11930 requires that the USP <61> test method is performed initially to ensure the product itself is free of microbial contaminants. Similar to the USP <51> methodology, which typically involves evaluations at 14 and 28 days, an additional sampling is performed at day 7. Depending on the performance of the cosmetic product demonstrated at each sampling interval, a determination can be made as to whether it meets Criteria A or Criteria B. The different criteria are intended to provide guidance to a manufacturer, based on how robustly-preserved a formulation is in its current state, how final packaging of the product can ensure consumer safety: a product that meets criteria A can be packaged in an open-faced jar or similar, while a product that meets criteria B should be used in a squeeze tube or similar to prevent contamination a consumer may introduce through normal use.
PCPC Microbiology guidelines m-3 Method for preservation efficacy testing of water-miscible personal care products
Established as an alternative to the USP <51> testing methodology with more stringent pass/fail criteria, The Microbiology Committee of the Personal Care Products Council (formerly known as the Cosmetics, Toiletries and Fragrance Association) generated their own guidelines through industry-wide collaborative testing. The M-3 method evaluates whether preservatives are effective in limiting contamination of water-miscible cosmetic products.
PCPC microbilogy guidelines m-6 method for preservative efficacy testing of atypical personal care products
Some personal care products are anhydrous and cannot be sampled using conventional methods. Those include oils, powders and wax-like products. Anhydrous products having a low water content may be considered “self-preserved” since microorganisms require water to grow. The M-6 method accommodates for challenges posed by testing these types of products.
PCPC MICROBILOGY GUIDELINES M-7 A SCREENING METHOD FOR PRESERVATION TESTING OF WATER MISCIBLE PERSONAL CARE PRODUCTS
The time from lab bench to market is crucial in a very competitive personal care product industry. This method is used to screen numerous preservative systems to help choose the most effective one for your formulation. This method does not replace the “M-3 Method for Preservative Efficacy Testing of Water-Miscible Personal Care Products” or the “USP <51> Antimicrobial Effectiveness Test”, but it does aid in identifying those systems that have a high probability of meeting the passing criteria for these methods.
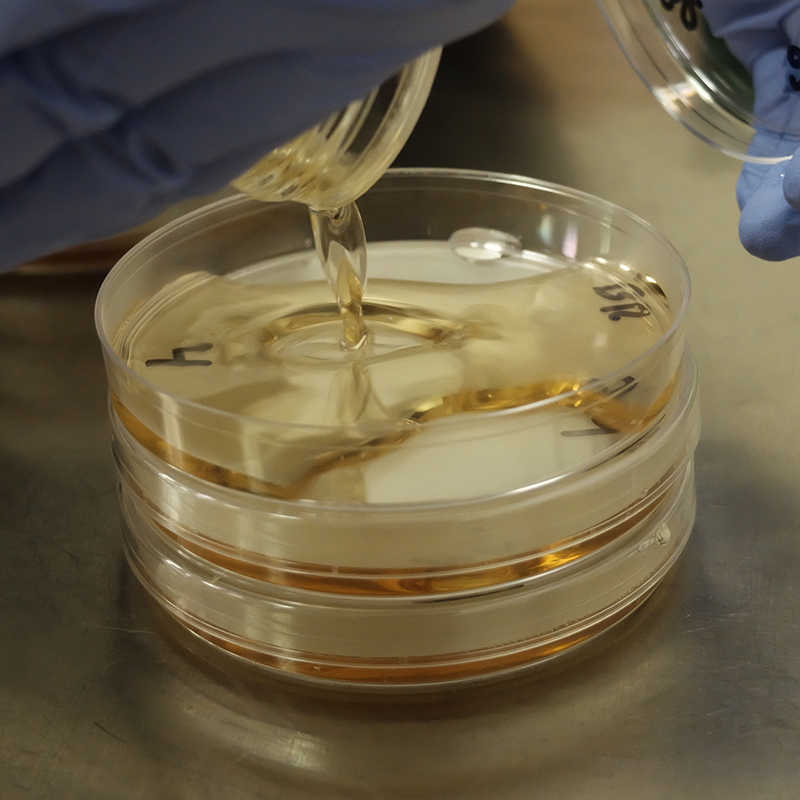
All the above mentioned methods involve the introduction of a controlled inoculum to test formulations. Test microorganisms include but are not limited to 5 different microorganisms, including 3 bacteria, 1 yeast and 1 fungus: Staphylococcus aureus, Escherichia coli, Pseudomonas aeruginosa, Candida albicans, and Aspergillus brasiliensis. These microorganisms are introduced to your formulation and sampling is performed to determine the number of surviving microorganisms at the defined sampling intervals. Based on the passing criteria of the specific test method followed, a specific log10 reduction in number of microorganisms recovered must be observed at certain time points in order to meet the passing criteria for the specific test method followed.
The usual experimental duration of these test methods is approximately 28 days for a single challenge. It is recommended that testing be performed on initial lab batch samples, artificially aged samples (preferably in the finished packaging), and on production samples in their finished packaging, which is important to ensure that there is no interaction between the preservative and the packaging material.
It should be noted that Antimicrobial Effectiveness Testing is not a replacement for GMP during the manufacturing process, but is used to ensure product safety/integrity while in the hands of the consumer.